Rewiring Hope and The Unexpected Ally in Your Brain's Fight Against Tumours
Brain tumours are abnormal growths of cells that develop within the brain or surrounding tissues. These tumours can be classified as either primary (originating in the brain) or secondary (metastatic, spreading from other parts of the body). Further classification includes benign (non-cancerous) and malignant (cancerous) tumours, with the World Health Organization (WHO) grading system categorizing tumours from grade I (least aggressive) to grade IV (most aggressive).
According to recent global cancer statistics, primary brain and central nervous system tumours account for approximately 2% of all cancers, with an estimated 308,000 new cases diagnosed worldwide in 2020. The incidence of secondary brain tumours is higher, affecting up to 40% of cancer patients with advanced disease.
The impact of brain tumours can be profound and varies depending on the tumour's size, location, and rate of growth. Common symptoms include headaches, seizures, vision problems, and cognitive impairments. However, symptoms can be more specific; for instance, tumours in the frontal lobe may cause personality changes, while those in the cerebellum can affect balance and coordination.
Diagnosis typically involves neurological examinations, advanced imaging techniques such as MRI and CT scans, and often requires a biopsy for definitive diagnosis and grading. Treatment usually requires a multidisciplinary approach involving neurosurgery, radiation therapy, and chemotherapy. Emerging therapies, such as immunotherapy and targeted molecular treatments, are showing promise in certain types of brain tumours.
Prognosis varies widely depending on factors such as tumour type, grade, location, extent of surgical resection, and the patient's age and overall health. While some low-grade tumours can be effectively managed, high-grade malignant tumours often carry a poor prognosis, highlighting the urgent need for continued research and development of new treatment strategies.
Causes and Risk Factors of Brain Tumours
Genetic Factors
Genetic factors play a significant role in brain tumour development. Inherited genetic syndromes account for about 5-10% of all brain tumours. Key examples include:
- Li-Fraumeni syndrome (TP53 gene mutation)
- Neurofibromatosis type 1 and 2 (NF1 and NF2 gene mutations)
- Tuberous sclerosis (TSC1 and TSC2 gene mutations)
- Von Hippel-Lindau syndrome (VHL gene mutation)
Sporadic genetic mutations, occurring without hereditary links, are more common. These often involve genes regulating cell growth and division, such as IDH1, IDH2, EGFR, and BRAF. Recent research has also identified epigenetic alterations as potential contributors to brain tumour development.
Environmental Factors
Radiation exposure is the most well-established environmental risk factor for brain tumours. Sources include:
- Therapeutic radiation for other cancers, particularly in childhood
- Diagnostic radiation (although the risk is much lower than therapeutic exposure)
- Occupational exposure in certain industries
Ionizing radiation can cause DNA damage, potentially leading to tumour formation. The risk increases with the dose and frequency of exposure.
Other environmental factors under investigation include:
- Electromagnetic fields from mobile phones (evidence remains inconclusive)
- Chemical exposures (e.g., pesticides, solvents), particularly in occupational settings
- Air pollution (emerging evidence suggests a possible link)
Lifestyle Factors
Obesity has been associated with an increased risk of certain brain tumours, particularly meningiomas. The proposed mechanisms include:
- Chronic inflammation
- Altered hormone levels
- Insulin resistance
Other lifestyle factors that may influence brain tumour risk include:
- Diet (high consumption of processed meats has been linked to increased risk)
- Physical activity (may have a protective effect)
- Alcohol consumption (limited evidence suggests a possible increased risk with heavy consumption)
Other Factors
Age is a significant risk factor, with brain tumour incidence generally increasing with age. However, certain types, like medulloblastomas, are more common in children.
Gender differences are observed in specific tumour types:
- Meningiomas are more common in females
- Glioblastomas are slightly more common in males
Racial and ethnic differences have also been noted, with higher incidence rates of certain tumours (e.g., meningiomas) in African Americans compared to other racial groups.
Immune System Factors
Immunosuppression, whether due to medical conditions (e.g., HIV/AIDS) or treatments (e.g., organ transplant medications), increases the risk of certain brain tumours, particularly central nervous system lymphomas.
Recent research has also highlighted the complex interplay between the immune system and brain tumour development. Chronic inflammation and altered immune surveillance may contribute to tumour formation and progression.
Symptoms of Brain Tumours
Brain tumours can cause a wide range of symptoms, which vary depending on the tumour's size, location, and growth rate. Symptoms can be categorized into general symptoms and location-specific symptoms.
General Symptoms
General symptoms are often caused by increased intracranial pressure due to the growing tumour. These symptoms may include:
- Headaches: Often worse in the morning or when lying down, and may not respond to over-the-counter pain medications.
- Nausea and vomiting: Particularly in the morning or with sudden movements.
- Seizures: Can range from focal seizures affecting a specific body part to generalized seizures involving the entire body.
- Vision changes: Including blurred or double vision, partial vision loss, or seeing flashing lights.
- Cognitive changes: Such as difficulty concentrating, memory problems, or confusion.
- Fatigue and drowsiness: Excessive sleepiness or difficulty staying awake.
- Balance and coordination issues: Including dizziness, vertigo, or difficulty walking.
- Personality or mood changes: Such as irritability, depression, or emotional instability.
Location-Specific Symptoms
Symptoms can also be specific to the location of the tumour within the brain:
1. Frontal lobe tumours:
- Personality changes
- Impaired judgment and decision-making
- Loss of motivation
- Language difficulties (if in the dominant hemisphere)
2. Temporal lobe tumours:
- Memory problems
- Hearing difficulties
- Seizures with unusual sensations or emotions
3. Parietal lobe tumours:
- Difficulties with spatial awareness
- Problems with reading or writing
- Numbness or weakness on one side of the body
4. Occipital lobe tumours:
- Visual field defects
- Difficulty recognizing objects or colors
5. Cerebellum tumours:
- Balance and coordination problems
- Unsteady gait
- Nystagmus (involuntary eye movements)
6. Brain stem tumours:
- Difficulty swallowing
- Facial weakness
- Double vision
- Breathing problems
Symptom Progression and Variability
It's important to note that brain tumour symptoms can:
- Develop gradually over time or appear suddenly
- Be constant or come and go
- Mimic other neurological or psychiatric conditions
- Vary in severity depending on the tumour's growth rate and the body's ability to adapt
Increased Intracranial Pressure
As a brain tumour grows, it can cause increased pressure within the skull, leading to additional symptoms such as:
- Persistent, severe headaches
- Papilledema (swelling of the optic disc)
- Altered level of consciousness
- In severe cases, herniation of brain tissue, which can be life-threatening
When to Seek Medical Attention
Early detection of brain tumours is crucial for effective treatment. Individuals should seek immediate medical attention if they experience:
- Sudden onset of severe headaches
- Seizures, especially if there's no history of epilepsy
- Sudden neurological deficits (e.g., weakness on one side of the body, vision loss)
- Persistent symptoms that worsen over time
Diagnosis of Brain Tumours
Diagnosing brain tumours involves a comprehensive approach combining clinical evaluation, imaging techniques, tissue analysis, and advanced molecular testing.
Neurological Examination
The initial step in diagnosis often involves a thorough neurological examination, which may include:
- Assessment of mental status and cognitive function
- Evaluation of cranial nerve function
- Testing of motor strength, sensation, and reflexes
- Coordination and balance tests
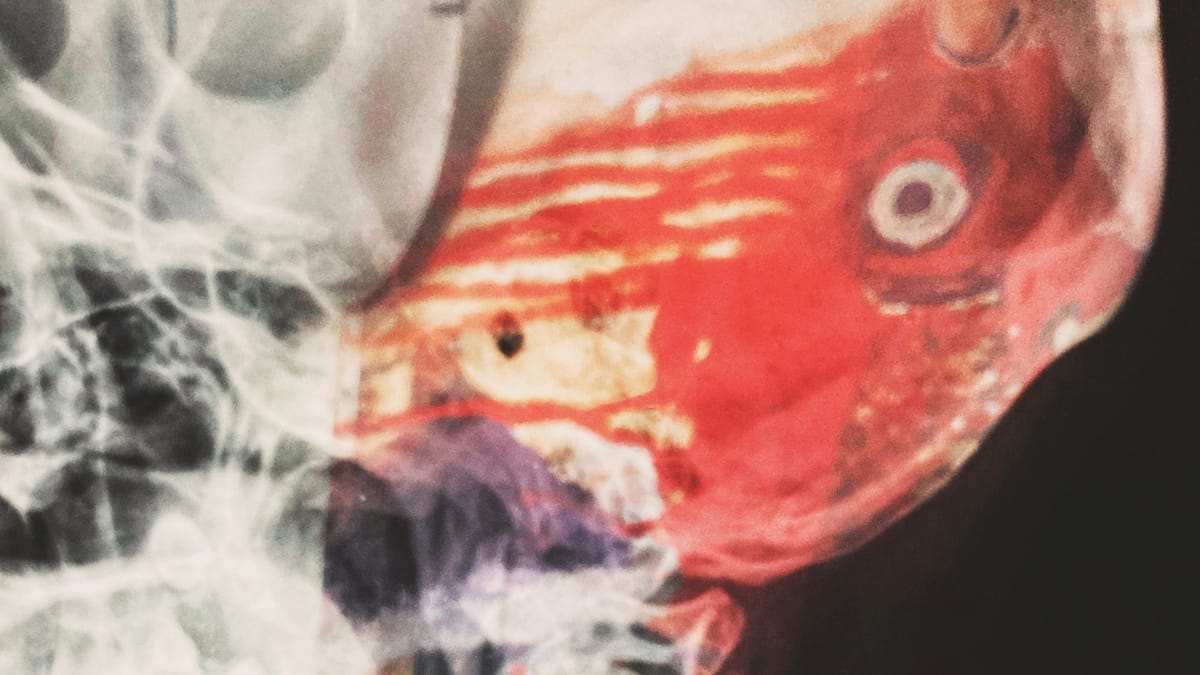
Imaging Techniques
Advanced imaging plays a crucial role in brain tumour diagnosis:
1. Magnetic Resonance Imaging (MRI):
Primary imaging modality for brain tumours
Provides high-resolution images of brain structure
Specialized MRI techniques include:
Diffusion-weighted imaging (DWI): Helps differentiate tumour types
Perfusion MRI: Assesses tumour blood supply
Magnetic Resonance Spectroscopy (MRS): Analyzes chemical composition of tumour tissue
2. Computed Tomography (CT):
- Often used for initial screening or in emergency situations
- Particularly useful for detecting calcifications and hemorrhage
- Less detailed than MRI for soft tissue contrast
3. Positron Emission Tomography (PET):
- Uses radioactive tracers to visualize metabolic activity
- Helps differentiate between tumour recurrence and radiation necrosis
4. Functional MRI (fMRI):
- Maps brain activity in relation to specific functions
- Useful for surgical planning to avoid eloquent areas
Biopsy and Histopathology
Tissue diagnosis remains the gold standard for brain tumour classification:
1. Stereotactic biopsy:
- Minimally invasive procedure using image guidance
- Suitable for deep-seated or multiple tumours
2. Open biopsy:
- Performed during surgical resection
- Allows for larger tissue samples
3. Histopathological analysis:
- Determines tumour type and grade based on WHO classification
- Involves microscopic examination of tissue architecture and cell morphology
Molecular and Genetic Testing
Advanced molecular diagnostics have become integral to brain tumour classification and management:
1. Immunohistochemistry:
- Identifies specific protein markers in tumour cells
2. Fluorescence In Situ Hybridization (FISH):
- Detects chromosomal abnormalities
3. Next-Generation Sequencing (NGS):
Identifies genetic mutations and alterations
Examples of important markers:
IDH mutation status in gliomas
MGMT promoter methylation in glioblastoma
1p/19q co-deletion in oligodendrogliomas
4. Methylation profiling:
- Provides detailed tumour classification based on epigenetic patterns
Additional Diagnostic Tools
1. Cerebrospinal Fluid (CSF) Analysis:
- May detect tumour cells or markers in CSF
- Particularly useful for certain tumour types (e.g., lymphoma, medulloblastoma)
2. Electroencephalography (EEG):
- Assesses electrical activity in the brain
- Useful for evaluating seizure activity associated with tumours
Emerging Technologies
1. Liquid biopsy:
- Analysis of circulating tumour DNA in blood or CSF
- Potential for non-invasive diagnosis and monitoring
2. Artificial Intelligence (AI) in imaging:
- Machine learning algorithms to assist in tumour detection and classification
The diagnostic process for brain tumours is complex and often requires a multidisciplinary approach. The combination of clinical assessment, advanced imaging, and molecular profiling allows for accurate diagnosis, which is crucial for determining the most appropriate treatment strategy and predicting prognosis.
Treatment Options for Brain Tumours
The management of brain tumours typically involves a multimodal approach, combining various treatment strategies tailored to the specific tumour type, grade, location, and patient factors. A multidisciplinary team of neurosurgeons, neuro-oncologists, radiation oncologists, and other specialists collaborates to develop the most effective treatment plan.
Surgical Interventions
Surgery remains a cornerstone of brain tumour treatment, with goals including:
1. Maximal safe resection:
Aims to remove as much tumour as possible without causing neurological deficits
Utilizes advanced techniques such as:
Intraoperative MRI for real-time imaging
Fluorescence-guided surgery (e.g., 5-ALA for high-grade gliomas)
Awake craniotomy for tumours near eloquent areas
2. Biopsy:
- For tumours in critical or inaccessible locations
- Stereotactic techniques for precise targeting
3. Debulking:
- Partial removal to relieve pressure and improve symptoms
- Often combined with other treatment modalities
4. Minimally invasive approaches:
- Endoscopic techniques for certain tumour types (e.g., pituitary adenomas)
- Laser interstitial thermal therapy (LITT) for small, deep-seated tumours
Radiation Therapy
Radiation therapy plays a crucial role in brain tumour management:
1. External beam radiation therapy (EBRT):
- Fractionated delivery over several weeks
- Intensity-modulated radiation therapy (IMRT) for complex tumour shapes
2. Stereotactic radiosurgery (SRS):
- Single high-dose treatment for small tumours
- Gamma Knife or linear accelerator-based systems
3. Proton beam therapy:
- Offers potential for reduced toxicity to surrounding tissues
- Particularly beneficial for pediatric tumours
4. Brachytherapy:
- Implantation of radioactive sources directly into the tumour
- Limited use in specific scenarios
Chemotherapy
Chemotherapy remains an important systemic treatment:
1. Temozolomide:
- Standard of care for glioblastoma
- Often used concurrently with radiation and as maintenance therapy
2. PCV regimen (procarbazine, lomustine, vincristine):
- Used in oligodendrogliomas and other gliomas
3. Platinum-based agents:
- Effective in certain pediatric brain tumours
4. Delivery methods:
- Oral administration
- Intravenous infusion
- Intrathecal delivery for leptomeningeal disease
- Local delivery (e.g., Gliadel wafers)
Targeted Therapy and Immunotherapy
Emerging treatments targeting specific molecular pathways or harnessing the immune system:
1. Targeted therapies:
- EGFR inhibitors (e.g., osimertinib) for EGFR-mutated glioblastoma
- BRAF inhibitors (e.g., dabrafenib) for BRAF-mutated tumours
- IDH inhibitors (e.g., ivosidenib) for IDH-mutant gliomas
2. Immunotherapies:
- Checkpoint inhibitors (e.g., pembrolizumab) under investigation
- CAR T-cell therapy in clinical trials
- Vaccine strategies (e.g., DCVax-L) showing promise
3. Antiangiogenic therapy:
- Bevacizumab for recurrent glioblastoma
Supportive Care and Symptom Management
Comprehensive care includes managing symptoms and treatment side effects:
- Anticonvulsants for seizure control
- Corticosteroids for peritumoral edema
- Pain management
- Cognitive rehabilitation
- Psychosocial support
Emerging Approaches
1. Tumor Treating Fields (TTFields):
- FDA-approved for newly diagnosed and recurrent glioblastoma
- Delivers alternating electric fields to disrupt cell division
2. Nanoparticle-based therapies:
- Enhanced drug delivery across the blood-brain barrier
3. Oncolytic virus therapy:
- Engineered viruses to selectively target tumour cells
Prognosis and Survival Rates
The prognosis for brain tumours varies widely depending on several factors. It's important to note that survival statistics are based on historical data and may not reflect the most recent advances in treatment. Individual outcomes can differ significantly from these general statistics.
Factors Affecting Prognosis
1. Tumour type and grade:
- Generally, low-grade tumours have a better prognosis than high-grade tumours
- Some tumour types (e.g., pilocytic astrocytoma) have a more favorable outlook than others (e.g., glioblastoma)
2. Tumour location:
- Tumours in accessible areas allowing complete surgical resection have a better prognosis
- Tumours in critical brain regions may limit treatment options
3. Extent of surgical resection:
- Greater extent of resection is generally associated with improved outcomes
4. Age at diagnosis:
- Younger patients often have a better prognosis than older patients
5. Patient's overall health and performance status:
- Better overall health is associated with improved tolerance of treatments and better outcomes
6. Molecular and genetic factors:
- Certain genetic markers are associated with better prognosis (e.g., IDH mutation, 1p/19q co-deletion in gliomas)
7. Treatment response:
- Initial response to treatment can be indicative of overall prognosis
Survival Rates for Common Brain Tumours
Survival rates are often expressed as 5-year relative survival, which compares the survival of people with brain tumours to those without. Here are approximate survival rates for some common brain tumours:
1. Glioblastoma (WHO Grade IV):
- 5-year relative survival rate: about 6.8%
- Median survival: 12-15 months with standard treatment
2. Anaplastic astrocytoma (WHO Grade III):
- 5-year relative survival rate: about 30%
3. Oligodendroglioma (WHO Grade II):
- 5-year relative survival rate: about 74%
4. Meningioma (typically benign):
- 5-year relative survival rate: over 80%
5. Medulloblastoma (pediatric tumour):
- 5-year relative survival rate: 60-70% overall, with variations based on subtype
6. Pituitary adenoma (typically benign):
- Generally good prognosis with appropriate treatment
Long-term Outcomes and Quality of Life
While survival is a crucial metric, quality of life is equally important:
- Many survivors experience long-term effects from the tumour or its treatment
- Cognitive changes, seizures, and hormonal imbalances may persist
- Rehabilitation and supportive care play key roles in optimizing functional outcomes
Recurrence and Follow-up
- Regular follow-up imaging and clinical assessments are crucial
- Some tumours have a high risk of recurrence, necessitating long-term monitoring
- Treatment options for recurrent tumours may be more limited
Emerging Prognostic Factors
Ongoing research is identifying new factors that may help refine prognosis:
1. Molecular profiling:
- Methylation patterns are providing more accurate tumour classification and prognostication
2. Liquid biopsy:
- Circulating tumour DNA may offer insights into treatment response and early detection of recurrence
3. Imaging biomarkers:
- Advanced MRI techniques may help predict treatment response and overall prognosis
Importance of Individualized Prognosis
It's crucial to emphasize that these statistics represent population-level data and may not accurately predict an individual's outcome. Each patient's situation is unique, and prognosis should be discussed in detail with the healthcare team.
Advances in treatment strategies, including targeted therapies and immunotherapies, are continually improving outcomes for many patients with brain tumours. Participation in clinical trials may offer access to promising new treatments.
While brain tumours remain a significant challenge, ongoing research and multidisciplinary care approaches are steadily improving both survival rates and quality of life for many patients."
Recurrence and Follow-Up
Brain tumour recurrence remains a significant challenge in neuro-oncology. Comprehensive follow-up care is crucial for early detection of recurrence and management of treatment-related effects.
Risk Factors for Recurrence
The likelihood of tumour recurrence varies widely and depends on several factors:
1. Tumour type and grade:
- High-grade tumours (e.g., glioblastoma) have a higher risk of recurrence
- Some low-grade tumours may transform to higher grades over time
2. Extent of resection:
- Residual tumour cells increase the risk of recurrence
- Complete resection, when possible, is associated with lower recurrence rates
3. Molecular and genetic factors:
- Certain genetic markers (e.g., IDH mutation, MGMT methylation) influence recurrence risk
- Molecular profiling helps in predicting recurrence patterns
4. Treatment history:
- Prior radiation may limit re-treatment options
- Development of treatment resistance can affect recurrence patterns
5. Location of the tumour:
- Tumours in areas allowing complete resection have lower recurrence risks
- Infiltrative tumours in eloquent brain areas pose challenges for complete removal
Follow-Up Care Protocol
A structured follow-up plan is essential for all brain tumour patients:
1. Imaging surveillance:
MRI is the gold standard for follow-up imaging
Frequency depends on tumour grade and time since treatment:
High-grade tumours: Every 2-3 months initially, extending to 3-6 months if stable
Low-grade tumours: Every 3-6 months initially, potentially extending to annual scans
2. Clinical assessments:
- Regular neurological examinations
- Cognitive function evaluations
- Quality of life assessments
3. Management of treatment-related effects:
- Monitoring and treating radiation necrosis
- Managing endocrine dysfunction in cases of pituitary involvement
- Addressing cognitive changes and fatigue
4. Psychosocial support:
- Regular screening for depression and anxiety
- Providing resources for coping and survivorship
Challenges in Monitoring Recurrence
1. Pseudoprogression:
- Treatment-related changes that mimic tumour progression on imaging
- Common after chemoradiation for high-grade gliomas
- Advanced imaging techniques (e.g., perfusion MRI, PET) may help differentiate
2. Radiation necrosis:
- Late effect of radiation that can be difficult to distinguish from tumour recurrence
- May require advanced imaging or even biopsy for definitive diagnosis
3. Multifocal recurrence:
- Some tumours may recur at sites distant from the original location
- Whole-brain imaging is crucial for comprehensive surveillance
Emerging Strategies in Recurrence Monitoring
1. Liquid biopsy:
- Analysis of circulating tumour DNA in blood or CSF
- Potential for early detection of recurrence and molecular evolution
2. Artificial Intelligence in imaging:
- Machine learning algorithms to assist in detecting subtle changes indicative of recurrence
3. Metabolic imaging:
- PET scans with specific tracers (e.g., amino acid PET) for improved detection of recurrence
Management of Recurrent Tumours
Treatment options for recurrent tumours may include:
- Re-resection when feasible
- Re-irradiation (considering cumulative dose limits)
- Systemic therapy (chemotherapy, targeted agents, or immunotherapy)
- Enrollment in clinical trials for novel therapies
Patient Education and Empowerment
- Educating patients about potential signs and symptoms of recurrence
- Encouraging open communication about new or worsening symptoms
- Providing resources for lifestyle modifications that may support overall health
Long-term Survivorship
For long-term survivors:
- Transitioning to less frequent imaging if stable over time
- Addressing late effects of treatment
- Managing the psychological impact of living with the risk of recurrence
Regular follow-up care is a critical component of brain tumour management. It allows for early detection of recurrence, timely intervention, and comprehensive care addressing both the physical and psychological needs of patients. As our understanding of brain tumour biology evolves and new monitoring technologies emerge, follow-up protocols will continue to be refined to provide optimal care for brain tumour survivors."
Research and Future Directions
The field of brain tumour research is rapidly evolving, with numerous exciting developments on the horizon. Current research priorities and future directions span a wide range of areas, from basic science to clinical applications.
Current Research Priorities
1. Molecular and Genetic Research:
- Single-cell sequencing to understand tumour heterogeneity
- Epigenetic profiling for improved tumour classification
- Identification of new therapeutic targets
- Understanding the role of the tumour microenvironment
2. Immunology and Immunotherapy:
- Enhancing immune system recognition of brain tumours
- Developing more effective CAR T-cell therapies
- Exploring combination approaches with checkpoint inhibitors
3. Precision Medicine:
- Integrating multi-omics data for personalized treatment planning
- Liquid biopsy development for non-invasive monitoring
- AI-driven predictive models for treatment response
4. Drug Delivery and Blood-Brain Barrier (BBB):
- Novel methods to enhance drug penetration across the BBB
- Nanoparticle-based delivery systems
- Focused ultrasound for temporary BBB disruption
5. Imaging Advancements:
- Development of novel PET tracers for improved tumour characterization
- AI-assisted image analysis for early detection and response assessment
- Integration of molecular and metabolic imaging
6. Quality of Life and Survivorship:
- Cognitive preservation strategies during treatment
- Managing long-term effects of therapy
- Psychosocial interventions to improve patient outcomes
Innovations in Treatment
1. Targeted Therapies:
- IDH inhibitors for IDH-mutant gliomas
- EGFR-targeted therapies for EGFR-amplified glioblastoma
- BRAF/MEK inhibitors for BRAF-mutated tumours
2. Immunotherapies:
- Personalized neoantigen vaccines
- Oncolytic virus therapies
- Bi-specific T-cell engagers (BiTEs)
3. Gene and Cell Therapies:
- CRISPR-based gene editing approaches
- Stem cell-based therapies for repair and regeneration
4. Combination Approaches:
- Rational combinations of targeted therapies, immunotherapies, and standard treatments
- Sequencing strategies to optimize treatment efficacy
5. Novel Radiotherapy Techniques:
- FLASH radiotherapy for reduced normal tissue toxicity
- Improved proton and heavy ion therapy delivery
6. Drug Repurposing:
- Investigating approved drugs for anti-tumour effects (e.g., metformin, statins)
Emerging Research Areas
1. Tumour Evolution and Clonal Dynamics:
- Understanding treatment resistance mechanisms
- Adaptive treatment strategies based on tumour evolution
2. Neurocognitive Mapping and Preservation:
- Advanced functional imaging for surgical planning
- Cognitive training interventions
3. Microbiome Research:
- Exploring gut-brain axis in tumour development and treatment response
4. Artificial Intelligence and Machine Learning:
- Predictive models for diagnosis, prognosis, and treatment planning
- AI-assisted surgical planning and intraoperative guidance
Clinical Trial Innovations
1. Adaptive Trial Designs:
- Platform trials to test multiple therapies simultaneously
- Basket trials based on molecular profiles rather than tumour type
2. Real-World Evidence:
- Integrating clinical trial data with real-world patient outcomes
3. Patient-Reported Outcomes:
- Increased focus on quality of life measures in clinical trials
Advocacy and Funding
1. Patient Advocacy:
- Increasing patient involvement in research prioritization
- Promoting access to clinical trials and novel therapies
2. Collaborative Networks:
- International consortia for data sharing and collaborative research
- Public-private partnerships to accelerate drug development
3. Funding Initiatives:
- Increased focus on high-risk, high-reward research
- Support for translational research to bridge lab discoveries and clinical applications
4. Policy and Regulatory Advancements:
- Efforts to streamline approval processes for brain tumour therapies
- Initiatives to improve access to novel treatments
Conclusion
Brain tumours represent one of the most formidable challenges in modern medicine, impacting not only the individuals diagnosed but also their families and communities. The complexity of these conditions, arising from the intricate structure and function of the brain itself, has long presented significant obstacles to effective treatment and management. However, as we've explored throughout this comprehensive overview, the landscape of brain tumour research and treatment is evolving rapidly, offering new hope and possibilities for patients and clinicians alike.
The journey from diagnosis to treatment and beyond is multifaceted, requiring a delicate balance of cutting-edge medical interventions and compassionate, patient-centered care. Recent advances in neuroimaging, molecular diagnostics, and surgical techniques have revolutionized our ability to detect, characterize, and treat brain tumours with increasing precision. The emergence of targeted therapies and immunotherapies, guided by our deepening understanding of tumour biology, is opening new avenues for personalized treatment strategies that promise improved efficacy and reduced toxicity.
Moreover, the holistic approach to brain tumour management now extends far beyond the initial treatment phase. Comprehensive follow-up care, including vigilant monitoring for recurrence and proactive management of treatment-related effects, has become integral to improving long-term outcomes and quality of life for survivors. The growing emphasis on survivorship care acknowledges the enduring impact of brain tumours and their treatment, addressing not only physical but also cognitive and psychosocial needs of patients throughout their journey.
The future of brain tumour research holds tremendous promise. From the exploration of novel drug delivery methods that can overcome the blood-brain barrier to the application of artificial intelligence in treatment planning and outcome prediction, the frontiers of innovation continue to expand. The integration of multi-omics data and advanced computational approaches is paving the way for truly personalized medicine, where treatment strategies can be tailored to the unique molecular profile of each patient's tumour.
However, the path forward is not without its challenges. The heterogeneity of brain tumours, the complexity of the central nervous system, and the persistent problem of treatment resistance all underscore the need for continued, intensive research efforts. Collaborative networks spanning academic institutions, pharmaceutical companies, and patient advocacy groups will be crucial in accelerating progress and translating scientific discoveries into tangible benefits for patients.
Importantly, the advancement of brain tumour research and treatment is not solely a scientific endeavor. It requires a concerted effort from multiple stakeholders, including policymakers, funding bodies, and the public. Increased awareness and advocacy are essential to securing the resources necessary for groundbreaking research and ensuring that all patients have access to the latest treatments and supportive care.
For individuals and families affected by brain tumours, this era of rapid scientific progress offers renewed hope. While the journey may still be challenging, the expanding array of treatment options, improved supportive care, and ongoing research initiatives provide reasons for optimism. Each new discovery, each clinical trial, and each improvement in patient care brings us one step closer to a future where brain tumours are more effectively managed, and perhaps one day, cured.
Thank you for reading this post!
If you found it helpful or informative, please consider sharing a 7 day free trial with your friends, family, or colleagues who might benefit from it.
Your support helps me reach more people and spread awareness on important topics like this. Together, we can make a difference!
Citations:
https://braintumourresearch.org/en-us/pages/information-brain-tumour-causes
https://www.cancercouncil.com.au/brain-cancer/symptoms/
https://www.moffitt.org/cancers/brain-cancer/diagnosis/risk-factors/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9777470/
https://www.hopkinsmedicine.org/health/conditions-and-diseases/brain-tumor/brain-tumor-treatment
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9161524/
https://www.cancerresearchuk.org/about-cancer/brain-tumours/treatment
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6827837/
https://www.nhs.uk/conditions/benign-brain-tumour/treatment/
https://www.cancer.org.au/cancer-information/types-of-cancer/brain-cancer
https://www.healthdirect.gov.au/brain-cancer
https://www.canceraustralia.gov.au/cancer-types/brain-cancer/awareness
https://www.mayoclinic.org/diseases-conditions/brain-tumor/symptoms-causes/syc-20350084
https://www.health.harvard.edu/a_to_z/brain-tumor-overview-a-to-z
https://www.mayoclinic.org/diseases-conditions/brain-tumor/diagnosis-treatment/drc-20350088
https://braintumourresearch.org
https://my.clevelandclinic.org/health/diseases/6149-brain-cancer-brain-tumor




