Flesh-Eating Nightmare: Japan's Battle Against a Silent Killer
Think about a disease that can turn a small scratch into a life-threatening emergency in just 48 hours. Now, picture this nightmare becoming reality for hundreds of people in one of the world's most advanced nations. Welcome to Japan's terrifying new reality.
In a twist that feels ripped from a sci-fi thriller, Japan is dealing with an unprecedented outbreak of what's nicknamed the "flesh-eating bacteria" disease, or, in its formal name, Streptococcal Toxic Shock Syndrome (STSS). But this isn't fiction – it's a very real and rapidly escalating health crisis that's sending shockwaves through the country and beyond.
As the land of cutting-edge technology faces this invisible enemy, the world watches. Could this be the first domino in a new global health scare? And what does it mean for you, no matter where you call home?
We will dive into the core of this medical disease, describing the story of a microscopic menace that's turning everyday cuts and scrapes into potential death sentences.
Epidemiology and Statistics: When Numbers Become Nightmares
If numbers could scream, Japan's latest health statistics would be setting off sirens worldwide. By June 2024, this island nation known for its longevity and health consciousness had logged a jaw-dropping 977 cases of Streptococcal Toxic Shock Syndrome.
The scale of the STSS outbreak in Japan has reached alarming proportions, with recent data painting a grim picture of its rapid spread. By June 2024, Japan had reported a staggering 977 cases of STSS, a figure that has not only surpassed but shattered the previous year's record high of 941 cases. This dramatic increase in such a short period has set off alarm bells within the medical community and public health sectors.
To put this surge into perspective, it's crucial to understand the historical context of STSS occurrences in Japan. In previous years, STSS cases were relatively rare, with annual numbers typically in the hundreds. The sudden spike to nearly a thousand cases midway through the year represents a significant departure from this trend, indicating a potential shift in the disease's prevalence or transmission patterns.
Now, brace yourself for the kicker: experts like Professor Ken Kikuchi, Japan's own version of a medical Nostradamus, are painting a future that's less rosy than a Kyoto spring. Their crystal ball shows a potential tsunami of 2,500 cases by year's end. That's not just a number – it's a national emergency in the making. Each of these cases isn't just a statistic; it's a person, a family, a community thrown into chaos.
The geographical distribution of cases adds another layer of complexity to the outbreak. While STSS cases have been reported across Japan, Tokyo has emerged as a particular hotspot for the infection. The concentration of cases in urban areas like Tokyo raises questions about the factors contributing to the spread, such as population density, lifestyle changes, or environmental conditions that might favor the proliferation of the causative bacteria.
The rapid increase in STSS cases is not just a matter of numbers; it represents a significant challenge to Japan's healthcare system and public health infrastructure. Each case requires intensive medical intervention, putting strain on hospital resources and medical personnel. Moreover, the potential for further spread poses a continuous threat to public health, necessitating a comprehensive and coordinated response from health authorities, medical professionals, and the public at large. Because in our interconnected global village, today's Japanese crisis could be tomorrow's worldwide wake-up call.
The Science of Scary: Understanding the Flesh-Eating Fiend
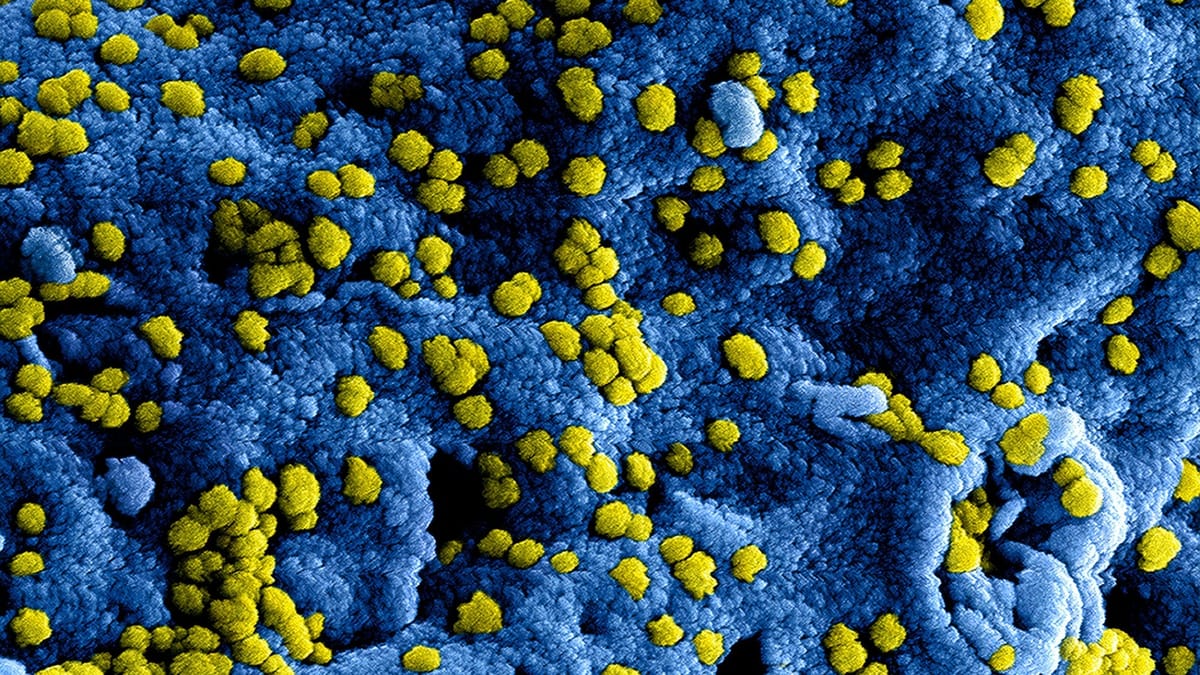
What we should worry about in this whole story is something called Group A Streptococcus (GAS), a bacterial threat with a habit of turning minor wounds into major catastrophes. This microscopic menace is the core behind Streptococcal Toxic Shock Syndrome (STSS).
Picture this, you nick yourself while cooking dinner. No big deal, right? Wrong. For the unlucky few, that tiny cut becomes ground zero for a bacterial invasion that moves very fast. Within hours, not days, victims can go from feeling a bit under the weather to fighting for their lives.
Here's the kicker, STSS doesn't discriminate, but it does have a favorite target. Data shows that the over-50 crowd is bearing the brunt of this bacterial blitzkrieg. This cohort appears to bear a disproportionate burden of this bacterial onslaught, suggesting a potential correlation between advancing age and increased susceptibility.
STSS distinguishes itself from conventional infections through its multifaceted assault on the human body. It manifests a constellation of alarming symptoms, including severe dermatological involvement, multi-organ dysfunction, and a paradoxical autoimmune response where the body's defense mechanisms appear to turn against itself.
The temporal dynamics of STSS progression are particularly concerning. In extreme cases, the interval between symptom onset and mortality can be as brief as 48 hours. This rapidity underscores the critical importance of timely intervention in STSS cases.
The statistical data surrounding STSS is sobering. Even with optimal medical management, mortality rates can reach up to 30%. This figure serves not merely as a statistic but as a clarion call echoing through Japan's medical institutions.
However, it is crucial to emphasize that knowledge and awareness are powerful tools in combating this condition. Recognition of early clinical signs – such as an unusually inflamed wound, persistent pyrexia, or pain of exceptional intensity – could be the determining factor between a narrow escape and a fatal outcome. In this high-stakes confrontation with a microscopic adversary, early detection is not merely important; it is potentially life-saving.
Global Alarm Bells: When Japan Sneezes, the World Catches a Cold
The bacterial fight unfolding in Japan has far-reaching implications beyond its national borders. As the nation grapples with this disease, the global community finds itself on high alert. The situation bears resemblance to a medical thriller unfolding in real-time, with nations worldwide speculating on their potential vulnerability.
Europe has already experienced its own encounters with STSS outbreaks, suggesting a pattern of transnational bacterial transmission that has captured the attention of health officials globally. The parallels observed are eliciting concern among public health experts worldwide, raising questions about the potential for similar outbreaks in diverse geographical locations.
An intriguing hypothesis posits that the COVID-19 pandemic may have inadvertently created conditions conducive to the emergence of STSS. As protective measures are relaxed and societies return to pre-pandemic norms, there is speculation that our immune systems, having been shielded from routine exposure to pathogens, may be more susceptible to opportunistic infections.
The quantitative aspects of this situation are noteworthy. While Japan braces for a potential 2,500 STSS cases this year, global health organizations are engaged in a complex process of epidemiological analysis. The 60 cases reported in England and sporadic occurrences in other European countries raise questions about whether these represent isolated incidents or harbingers of a more widespread phenomenon.
The World Health Organization, ever vigilant in the face of potential health crises, has focused its attention on this necrotizing bacterial threat. Their efforts encompass case tracking, data analysis, and strategic planning to address the potential for a global STSS outbreak. This situation serves as a poignant reminder of the interconnectedness of global health, where a localized outbreak can have far-reaching consequences.
It is crucial, however, to approach this situation with informed caution rather than undue alarm. Japan's ongoing battle against STSS serves as an invaluable case study for the global medical community. Each treatment protocol, preventive strategy, and clinical success contributes to a growing body of knowledge that can inform global health systems.
As the scientific community intensifies its research efforts and health officials engage in urgent consultations, one fact becomes increasingly clear: STSS is no longer an isolated concern but a global health challenge. Whether in Osaka or Oslo, the imperative remains consistent: maintain vigilance, adhere to hygiene protocols, and approach even minor wounds with due caution.
The Sushi Master's Smallest Cut: Haruki's Battle with STSS
Haruki Tanaka, a 55-year-old sushi chef in Tokyo, had always prided himself on his precision knife skills. His hands, calloused from years of slicing fish, were his most valuable tools. One busy Friday evening, as he prepared an intricate platter for a group of food critics, the unthinkable happened. His knife slipped, leaving a small cut on his index finger.
"Just a scratch," Haruki muttered, quickly wrapping a bandage around it before returning to work. He couldn't afford to lose time, not with the restaurant buzzing and his reputation on the line.
By Saturday morning, Haruki's finger throbbed with an intensity he'd never experienced. An angry red streak had begun creeping up his arm. Still, he pushed through the discomfort, chalking it up to a long week and lack of sleep.
Sunday arrived, and with it came a fever that left Haruki shivering despite the summer heat. His wife, alarmed by his rapidly deteriorating condition, insisted on taking him to the hospital. It was there that the gravity of the situation became clear.
"Streptococcal Toxic Shock Syndrome," the doctor said gravely, her words cutting through Haruki's feverish haze. "It's critical we begin treatment immediately."
The next 48 hours were a blur of antibiotics, surgeries, and anxious waiting. Haruki's seemingly innocuous cut had opened the door to a life-threatening infection that was now racing through his body.
As he lay in the ICU, machines beeping around him, Haruki reflected on the irony. Years of handling raw fish without incident, only to be felled by a tiny slip of the knife. He vowed that if he survived this ordeal, he would become an advocate for STSS awareness in the culinary community.
Thankfully, due to early intervention and aggressive treatment, Haruki made a full recovery. True to his word, he now starts each shift with a reminder to his staff about the importance of properly treating even the smallest kitchen injuries. His experience serves as a sobering reminder that in the world of flesh-eating bacteria, vigilance can mean the difference between life and death.
Your Top Questions Answered
What is Streptococcal Toxic Shock Syndrome (STSS)?
Ivermectin is a widely used antiparasitic drug that has been used to treat a variety of parasitic infections, including river blindness, scabies, and lice infestations.
Who is most at risk for STSS?
While STSS can affect anyone, data suggests that individuals over 50 years of age are at higher risk. However, it's important to note that people of all ages can potentially develop STSS if exposed to the causative bacteria.
What are the early signs and symptoms of STSS?
Early signs include:
- Unusually inflamed or painful wounds
- Persistent high fever
- Intense pain that seems disproportionate to the visible injury
- Rapid progression of symptoms
Is STSS related to the COVID-19 pandemic?
While there's no direct causative link, some experts speculate that the COVID-19 pandemic may have created conditions that could increase susceptibility to infections like STSS. This could be due to changes in immune system responses following prolonged periods of reduced exposure to common pathogens during lockdowns and social distancing.
Is STSS a global threat?
While the recent outbreak has been most prominent in Japan, STSS cases have been reported in other countries, including parts of Europe. The World Health Organization is monitoring the situation closely due to its potential for cross-border spread. However, it's important to maintain perspective – while serious, STSS is still relatively rare compared to many other infectious diseases.
How to get streptococcal toxic shock syndrome?
Streptococcal toxic shock syndrome (STSS) is contracted when group A streptococcus bacteria invade the body through breaks in the skin or mucous membranes. This can occur due to minor cuts, surgical wounds, or underlying infections, leading to a rapid and severe systemic reaction.
What happens if you get toxic shock syndrome?
If someone contracts toxic shock syndrome, they may experience a sudden onset of symptoms such as high fever, chills, confusion, a rash resembling a sunburn, nausea, vomiting, diarrhea, and muscle aches. In severe cases, low blood pressure, organ failure, and even death can occur without prompt treatment.
What is the cause of streptococcal shock syndrome?
Streptococcal shock syndrome is primarily caused by toxins released by group A streptococcus bacteria. These toxins can trigger a massive immune response, leading to widespread inflammation and damage to multiple organ systems, which is what characterizes this severe form of bacterial infection.
How long does a tampon have to be in to get TSS?
While there's no definitive duration, leaving a tampon in place for more than eight hours can increase the risk of developing toxic shock syndrome, especially if the tampon has a high absorbency level. This is typically associated with another type of bacteria, Staphylococcus aureus, rather than group A streptococcus.
Can I get TSS from pulling out a dry tampon?
It is uncommon to develop toxic shock syndrome simply from removing a dry tampon. However, if the removal causes trauma or introduces bacteria into the genital tract, there could be a risk of infection that might lead to TSS under certain conditions.
Who is most likely to get streptococcal toxic shock syndrome?
Those most susceptible to streptococcal toxic shock syndrome include individuals who use super-absorbent tampons, people with open wounds or recent surgeries, immunocompromised individuals, and those with a previous history of TSS. Pregnant women and postpartum women also have an increased risk.
Is streptococcal toxic shock syndrome curable?
Streptococcal toxic shock syndrome is indeed curable, but early recognition and immediate medical intervention are critical. Treatment typically involves antibiotics to combat the bacterial infection, supportive care to manage symptoms, and sometimes surgery to remove infected tissue.
How common is sepsis from strep throat?
Sepsis arising from strep throat is relatively uncommon since strep throat is generally a less severe infection. However, if left untreated or in cases where the infection becomes particularly aggressive, strep throat can progress to serious complications such as sepsis, which is a life-threatening condition characterized by a body-wide inflammatory response to infection.
Key Takeaways
- Pathogen Identification: Group A Streptococcus (GAS) is identified as the primary causative agent of Streptococcal Toxic Shock Syndrome (STSS), emphasizing its ability to transform minor wounds into severe medical emergencies.
- Rapid Progression: STSS is characterized by its alarmingly swift progression, with patients potentially transitioning from mild symptoms to life-threatening conditions within hours rather than days.
- Age-related Vulnerability: While STSS can affect anyone, individuals over 50 years of age appear to be disproportionately impacted, suggesting a potential correlation between advancing age and increased susceptibility.
- Multisystem Impact: STSS distinguishes itself through its multifaceted assault on the body, causing severe dermatological involvement, multi-organ dysfunction, and paradoxical autoimmune responses.
- High Mortality Rate: Even with optimal medical care, STSS carries a mortality rate of up to 30%, underscoring the severity of the condition and the urgent need for effective treatments.
- Global Implications: The STSS outbreak in Japan has raised international concerns, with similar cases reported in Europe, highlighting the potential for cross-border transmission and global health implications.
- COVID-19 Connection: There's speculation that the COVID-19 pandemic may have inadvertently created conditions conducive to STSS emergence, possibly due to altered immune responses following prolonged periods of reduced pathogen exposure.
- Early Detection Criticality: Recognizing early signs of STSS, such as unusually inflamed wounds, persistent fever, or intense pain, is crucial for improving patient outcomes.
- World Health Organization Involvement: The WHO is actively monitoring the STSS situation, tracking cases and analyzing data to prepare for potential global outbreaks.
- Learning Opportunity: Japan's ongoing battle against STSS serves as a valuable case study for the global medical community, providing insights into treatment protocols, preventive strategies, and clinical management of the condition.
Thank you for reading this post!
If you found it helpful or informative, please consider sharing a 7 day free trial with your friends, family, or colleagues who might benefit from it.
Your support helps me reach more people and spread awareness on important topics like this. Together, we can make a difference!
References
https://www.theguardian.com/world/2024/mar/15/japan-streptococcal-infections-rise-details
https://www.cdc.gov/groupastrep/diseases-public/streptococcal-toxic-shock.html
https://www.who.int/news-room/fact-sheets/detail/streptococcal-infections
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7387263/
https://www.nejm.org/doi/full/10.1056/NEJMra1804564
https://www.sciencedirect.com/science/article/abs/pii/S1198743X19303592
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(19)30532-8/fulltext
https://www.nature.com/articles/s41579-018-0112-x
https://www.cdc.gov/abcs/reports-findings/survreports/gas14.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6183474/
https://www.sciencedirect.com/science/article/abs/pii/S1198743X19303592
https://www.who.int/news-room/fact-sheets/detail/streptococcal-infections
https://www.cdc.gov/groupastrep/diseases-public/necrotizing-fasciitis.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6183474/
https://www.nejm.org/doi/full/10.1056/NEJMra1804564
This article was written by Ariadna Paniagua, an experienced writer and editor for several institutions, papers, and websites.




